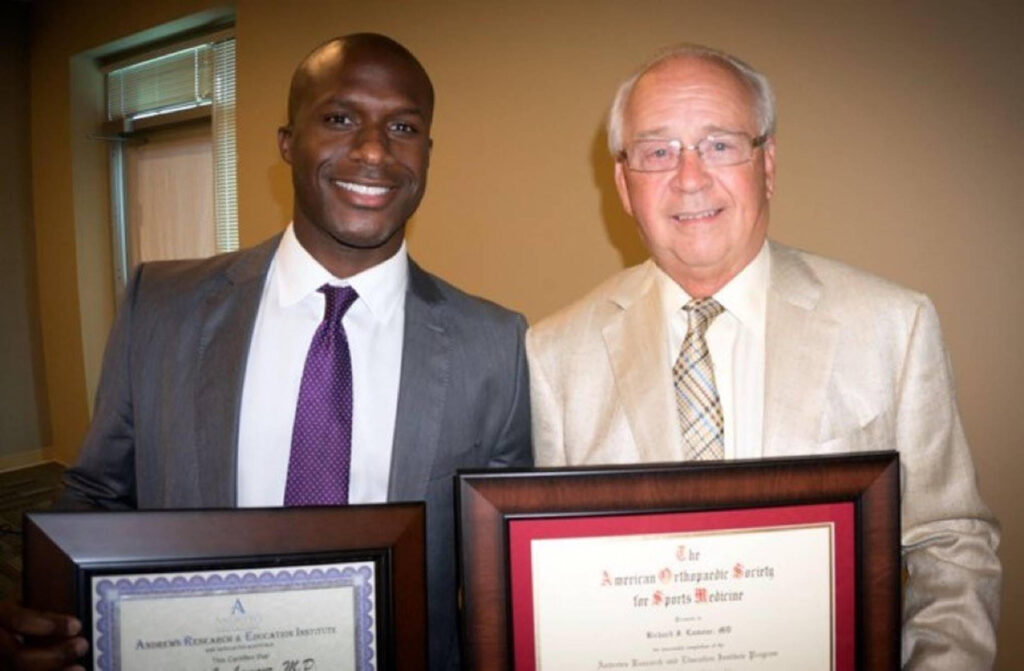
Richard J. Lamour, M.D. is a dual-fellowship-trained, board-certified orthopaedic surgeon specializing in the lower extremities as well as sports medicine. Previously, Dr. Lamour provided medical care to the University of Miami football team, the Miami Marlins baseball team, the Auburn University football team, and the Fresno State basketball team. In this interview, Dr. Lamour talks about the value of social media for physicians, the latest bunion correction options, and why each patient need a customized care plan.
Can you tell me about the focus of your work at OOA?
I’m a knee, ankle, and foot specialist. I’m also trained in sports medicine. As far as knee injuries, I see anterior cruciate ligament (ACL) and meniscus injuries. For the ankle and foot, I see the gamut. I do everything from fractures to deformity correction, arthritis to ankle sprains, Achilles ruptures, cartilage injuries, ankle replacements, ankle and foot fusions, and bunion corrections.
What does sports medicine involve?
When people think of sports medicine, they often think of athletes or sports teams. But sports medicine applies to everyday folks, because at the end of the day everyone is sort of like an athlete with the way they approach their daily life. So I offer the same things to athletes as to everyone else. People need to get back to work quickly just like athletes need to get back to the game and similar concepts apply to anybody trying to get back to work or the recreational things that they love to do.

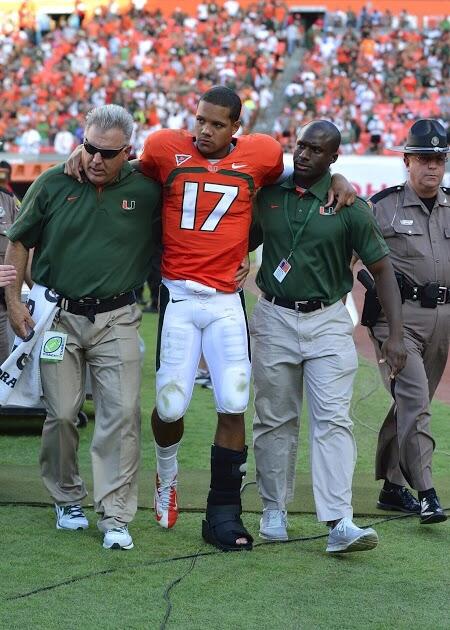
How did your time providing medical care to major sports teams inform your current practice?
It has helped a lot because I picked up a lot of tools from working with athletes and tips from all the folks that I was mentored by. I learned how to care for high-level athletes and then how to take that level of treatment and transfer it to non-athletes too.
It was very helpful to have that experience in order to bring cutting edge treatment to patients in our area. A lot of patients are appreciative that I’m able to offer them the latest technology and techniques that maybe they haven’t been offered before.
Meet Our Foot & Ankle Team
Can you tell me about some of the community outreach the OOA sports med team does with local sports teams?
Our sports medicine team includes doctors and athletic trainers. We provide sports medicine coverage to most of the high schools and local colleges in our area. That means attending games, going to athletic training rooms, and providing more expedient and direct care to athletes.
We do this for particularly for football, which is a sport where kids get injured fairly routinely throughout the game. Most of the injuries are minor and can get evaluated and cleared on the sidelines. For those injuries that a player cannot be cleared for, they’re out. So it’s vital to have people on the sidelines to make medical decisions so coaches or other support staff are not having to do so.
What are some reasons why a patient would require reconstructive ankle surgery?
Arthritis is the most common reason for reconstructive ankle surgery. Usually there are some trauma years before and then as time passes, arthritis has settled in. Arthritis can bring pain and deformity because the joint wears in a certain pattern that causes the ankle to turn in or turn out.
Tell me about your new approach to bunion correction surgery.
I’ve adopted a new approach in the last few months. It’s a more minimally invasive approach with new technology and it’s a game changer. The idea is that we’re doing similar things as before – making bone cuts, then shifting and realigning the bones that are out of position. But traditionally, we’d have to make large incisions to access the bones and visualize everything. Now, we’re able to do this through small keyhole incisions using a special burr unit that cuts the bone but not any of the soft tissues. These cuts are made under x-ray guidance so we can do them without having to make large incisions to visualize directly.
Previously, I’ve had patients who have come for a bunion surgery and then come back and say, “Alright, this is a little more than I expected. I’m going to wait to do the other side.” Or they might not do the other side ever. But with this new approach, I’ve already had a patient come back at just eight weeks’ postop feeling really good and ready to get the other side done! That is the kind of response that I’m getting – a lot of these patients are doing really well.

What is your favourite thing about OOA?
My favourite thing about working here is the fact that everyone has the same mindset and the same goal: we want to deliver efficient and exceptional care to patients. And it’s also a very friendly and family-oriented environment.
In 2019, an NCBI study listed you among the top 100 social media influencers in orthopaedic surgery. Why have you chosen to have an active presence, as a surgeon, on social media?
I love using social media because I get to communicate with my colleagues on a very direct level. It’s much easier than just seeing them at conferences or just communicating with them through journals. Social media can be a learning tool, honestly, in addition to medical journals I read. I see what others are posting on social media from a journal or about a case they did. From that standpoint, the collaborative effects of social media are awesome.
On top of that, I feel that it shows patients that I’m still active and have a presence in orthopedic sports medicine. I work hard to stay on top and be cutting-edge as far as the newest things that are available, so I love seeing new products that companies or other providers have used and posted about.
Do your patients ever find you on social media?
I’ve had patients who have chosen to connect with me on social media. I can think of one patient who was a college athlete who ruptured his Achilles tendon towards the end of the season. We ended up fixing it, getting him back in the game and now he has gone on to play in the NFL. He’s an avid social media user so he’s always posting on social media about his workouts and what he is doing to recover now. He just signed with a professional team the other day so it was fun to message with him. I look forward to following him on social media and on TV.
If other surgeons are thinking of building a social media presence, are there any HIPAA regulations challenges they should be aware of?
It’s something I’m still learning, but really it’s just a matter of always getting approval from a patient before posting. Most things, like x-rays or MRIs, can be completely de-identified or you can post a video of a knee motion with the face blurred out, but you always need the patient’s consent. Those things are all doable and let you connect with your peers online. It also helps patients see that you’re active. Because when patients search for you online – because they will – if there is almost nothing there or just some random reviews, then there’s a little bit less of a presence for them to get to know you before meeting you.
Finally, what can patients expect when they come see you?
I make a very deliberate effort to listen to patients and formulate a patient-specific plan. No plan is the same from patient to patient. I try and do everything I can to get the patient the outcome they want on their terms.
It seems that everyone comes to my office at a different point in their disease process. Some patients have already gone through all the non-surgical treatments and want surgery. Some people are wanting to avoid surgery altogether. And some people just can’t have surgery because they’re not great surgical candidates. So I do everything I can to treat them non-surgically, even if that means that we have to ‘abridge the textbook’ to make it work for the patient. Basically, I want patients to know that I’m willing to work with them to get the outcome that they want.
