Understanding Degenerative Disc Disease (DDD)
Degenerative disc disease (DDD) is a common spinal condition that affects millions of people, often causing chronic neck pain or back pain. Despite its name, DDD isn’t actually a “disease” but rather a natural part of aging and normal degeneration of the spine. Understanding what causes this condition, how it presents, and the range of treatment options available can empower patients to take an active role in managing their spinal health. This article will walk you through what you need to know about DDD and how you can find relief.
What Is Degenerative Disc Disease?
Degenerative disc disease refers to the breakdown of the intervertebral discs that cushion the bones (vertebrae) in your spine. These discs act like shock absorbers, allowing flexibility and movement in the spine. Over time, these discs dry out, bulge, shrink in height and become more rigid, which reduces their ability to function effectively. As the discs deteriorate, they can cause pain, stiffness, and reduced mobility. In some cases, disc degeneration may lead to other spinal conditions such as spinal stenosis.
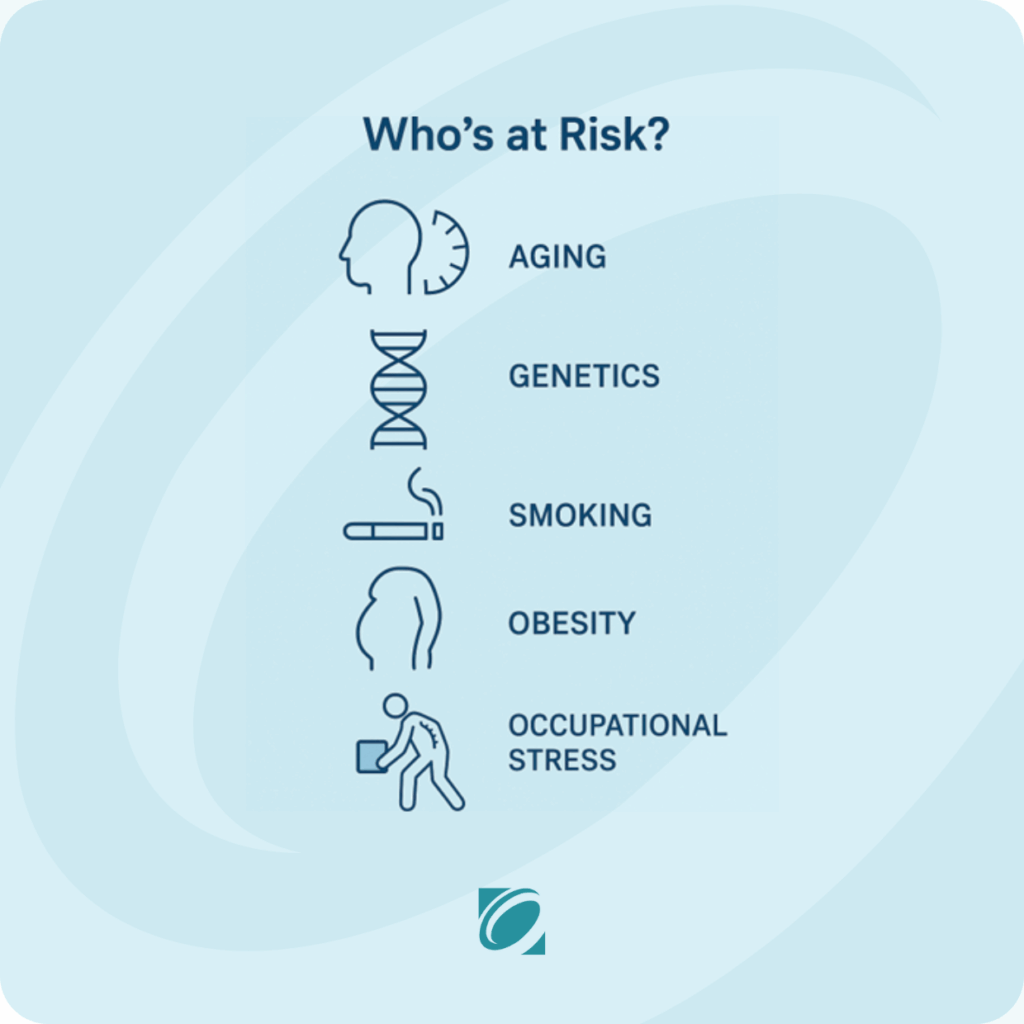
Causes and Risk Factors
DDD is part of the natural aging process, but injury or prior trauma to a disc (“herniation”) can predispose a person to more disc degeneration. Other risk factors can also increase your likelihood of developing DDD, such as such as smoking or having family history of spinal problems.
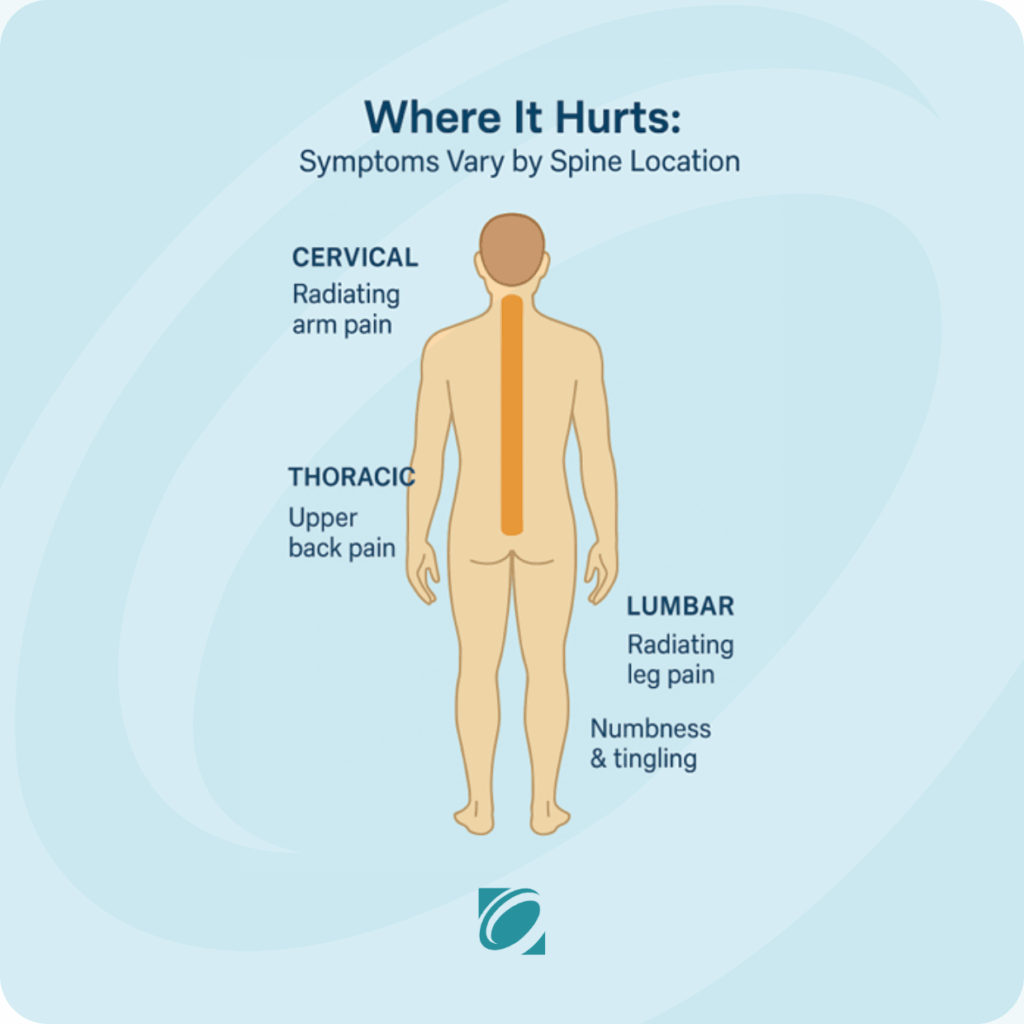
Recognizing the Symptoms
Symptoms of degenerative disc disease can vary depending on the severity and location of the degeneration. Common complaints include chronic neck pain or back pain, especially when sitting, bending, or lifting. In the cervical spine (neck), symptoms might be felt in the shoulders and arms, while in the lumbar spine (lower back) symptoms might radiate to the hips, buttocks, and legs. If the nearby nerve roots are compressed, patients might also experience numbness, tingling, or weakness in the arms or legs. Thoracic spine disc degeneration, though often less symptomatic, can also cause significant discomfort.
Diagnostic Procedures
Evaluating DDD typically begins with a review of your medical history and symptoms, as well as a physical examination to assess mobility, strength, and neurological function. Imaging studies play a crucial role in confirming the diagnosis and understanding the extent of disc damage. Imaging studies, such as X-rays, MRI scans and CT scans can reveal disc space narrowing and other degenerative changes.
Treatment Options
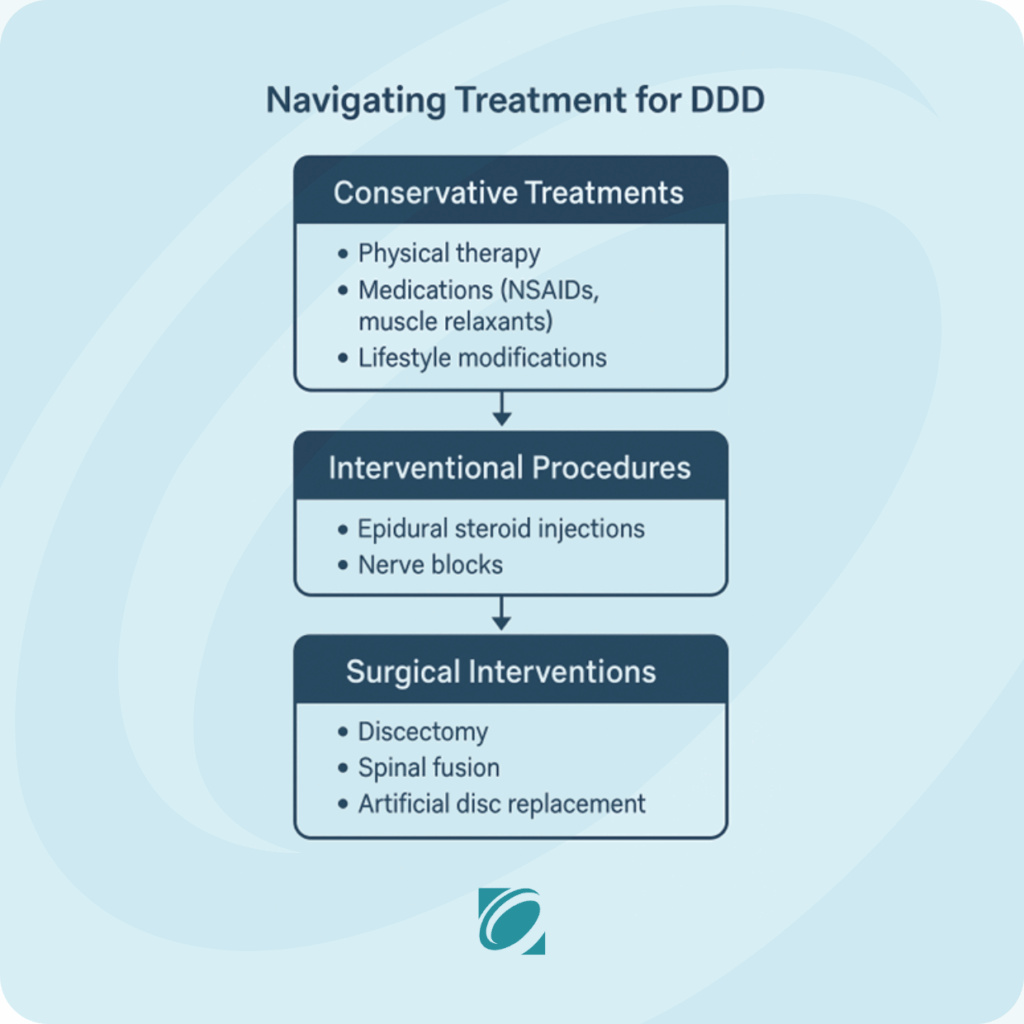
Treatment for degenerative disc disease focuses on relieving pain and improving function. Options range from non-invasive therapies to advanced surgical procedures, depending on the severity of symptoms and a patient’s response to initial care.
Conservative Treatments
The first line of treatment often includes physical therapy aimed at strengthening core muscles and improving spinal stability. Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants can provide symptom relief. Lifestyle changes—like maintaining a healthy weight, practicing good posture, and avoiding tobacco use—are also crucial. Alternative therapies such as acupuncture, massage, and chiropractic care may complement traditional approaches and provide additional relief for some patients.
Interventional Procedures
If conservative treatments are insufficient, interventional options may be recommended. Epidural steroid injections can reduce inflammation and provide temporary pain relief in some patients, especially those with symptoms radiating into the arms and legs. Nerve blocks and other non-surgical interventions can be used to decrease pain and improve function.
Surgical Interventions
Surgery may be considered when non-surgical treatments fail to provide adequate relief or when neurological symptoms worsen. Common procedures include discectomy (removal of a portion of a herniated disc), spinal fusion (joining two or more vertebrae to eliminate motion and pain), and artificial disc replacement (inserting a prosthetic disc to preserve mobility). Surgical candidates are carefully selected based on symptoms, a physical examination, imaging findings, functional limitations, and overall health status. Many patients experience significant pain reduction and improved quality of life following surgery.
Living with Degenerative Disc Disease
Managing degenerative disc disease is often a lifelong commitment that involves both medical support and personal effort. Incorporating ergonomic adjustments at work and home—such as using lumbar support or adjusting screen height—can ease daily strain on the spine. Regular low-impact exercise like walking, swimming, or yoga can strengthen muscles and enhance flexibility. Your personal treatment plan can be adjusted as needed with periodic follow-up with your healthcare provider. By being informed and proactive, patients with DDD can lead active, fulfilling lives despite their diagnosis.
Think This Sounds Like You?
If these symptoms hit a little too close to home, you don’t have to power through the pain alone. Our orthopaedic specialists can help diagnose the root cause of your discomfort and create a personalized plan to address your back pain.
- Same-week appointments often available
- Expert diagnosis and tailored treatment plans
- Non-surgical and surgical options to fit your needs
Schedule your evaluation today and take the first step toward lasting relief.
Book Online or call us at (360) 570-3460
This information has been medically reviewed by Dr. Zachary Abbott, D.O., a board-certified physiatrist at Olympia Orthopaedic Associates.